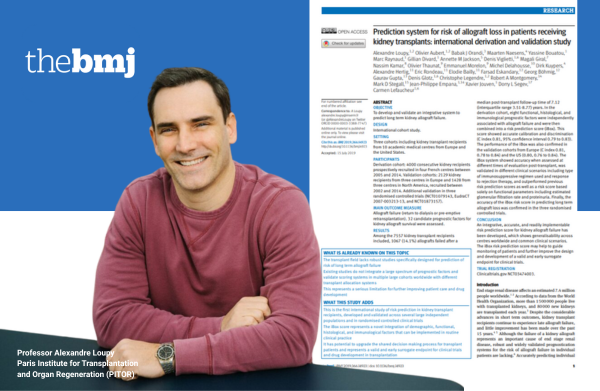
A rich history with global impact
Since 1840, BMJ Group has supported health professionals in improving patient outcomes worldwide.
Today, as a global healthcare knowledge provider, our vision of helping to create a healthier world lies at the heart of everything we do.
For BMJ Group, impact means driving positive, measurable change across the entire healthcare ecosystem. It’s about enabling better healthcare outcomes by delivering the best available and most credible research and evidence based policy guidelines. It’s also about fostering a skilled and supported workforce.
In essence, for our values driven organisation, impact is about creating a ripple effect where better knowledge, supported health professionals, and accessible evidence of the highest standard work together to improve individual patient outcomes and the broader health systems worldwide.

As deputy editor of this important journal from the BMJ Group, I can’t help but to stress both the educational importance of case reports, but also their role in shaping often important public health advices.
Rui Amaral Mendes
Professor of the Department of Community Medicine, Case Western Reserve University, Cleveland, Ohio, United States
Spotlight on safety
Sometimes it takes just a single clinical observation to make the world sit up and listen.
When Dr Clara Maarup Prip at Aarhus University Hospital submitted a case report to BMJ Case Reports about a rare complication from menstrual cup use (kidney swelling caused by ureter compression), she didn’t expect it to go viral. Yet within weeks, it had been reported by 23 major news outlets, sparked four opinion pieces, and triggered public health advice across multiple countries.
📊 25,000+ views in the first month
📰 29 media stories worldwide
🌍 Top 5% of all research outputs by Altmetric score
📽️ Prompted safety advice and “how-to” resources in major media outlets
It’s a striking reminder that impact isn’t only measured in citations. Case reports like this can directly change behaviour, guide safer use of everyday products, and even shape public health conversations.
We weren’t funded, and it didn’t take long to write. But the response shows just how much value a single case report can bring.”
Dr Clara Maarup Prip
Urologist and gynaecologist, Aarhus University Hospital, Denmark
Championing the rights and health of street and working children
Millions of children live and work on the streets, exposed to violence, exploitation and exclusion. Under Professor Shanti Raman’s leadership, the global Street and Working Children Working Group is tackling this head on by creating tools, advocacy resources and evidence to protect their health and rights.
BMJ Paediatrics Open plays a vital role in this mission. Its special collection on Street and Working Children features published papers that give health professionals and policy makers rigorous, evidence informed research and practical tools to address the complex needs of street and working children.
It also ensures children’s own voices are heard through their stories and aspirations shared with health professionals, policy makers and global audiences.
Flour fortification with folic acid – a landmark decision for public health
The UK government has officially announced the mandatory fortification of flour with folic acid, a transformative policy to prevent neural tube defects (NTDs) in newborns. This decision comes after years of advocacy and mounting scientific evidence supporting the measure as a cost-effective way to improve public health.
Experts like Professor Sir Nicholas Wald have been advocating for this policy. In a June 2024 opinion piece published in The BMJ, Wald argued that fully effective fortification could prevent up to 80% of NTDs, compared to the current approach of relying on individual supplementation, which reaches far fewer people.
This government announcement reflects the recommendations of numerous health experts and organisations, including the scientific consensus on the safety and efficacy of fortification.
Advocating for safer pharmaceutical marketing
Nearly 90% of teens and young adults who use social media say they use it to find information about their healthcare. However, as pharmaceutical marketers have shifted more and more of their budgets towards selling their products on social media, especially via paid influencers, the US Food and Drug Administration’s (FDA) regulation has lagged behind.
A new landmark legislation, The Protecting Patients from Deceptive Drug Ads Online Act, introduced by Senators Durbin (D-IL) and Braun (R-IN), directs the FDA to update and enforce its regulations for promoting prescription drugs on social media. It does this by focusing the agency’s attention specifically on deceptive or misleading communications by telehealth companies, social media influencers, and health providers.
This act is a direct result of the work of Generation Patient, led by its founder and BMJ patient advisor, Sneha Dave. This legislation was particularly noteworthy because it was heavily influenced by patient advocacy, especially from a young patient group. It’s not often that patients lead the charge for legislation like this.