Improving allied health decision making to reduce readmissions
Hospital readmissions place sustained pressure on inpatient services and are frequently influenced by modifiable factors, including how patients are identified for targeted allied health input. Observational studies have shown that higher hospital investment in occupational therapy is associated with lower readmission rates, indicating that allied health decision making contributes to reducing avoidable returns to hospital. National workforce reviews have also highlighted that enabling clinicians to work at full scope of practice improves resource use and service efficiency within constrained systems.
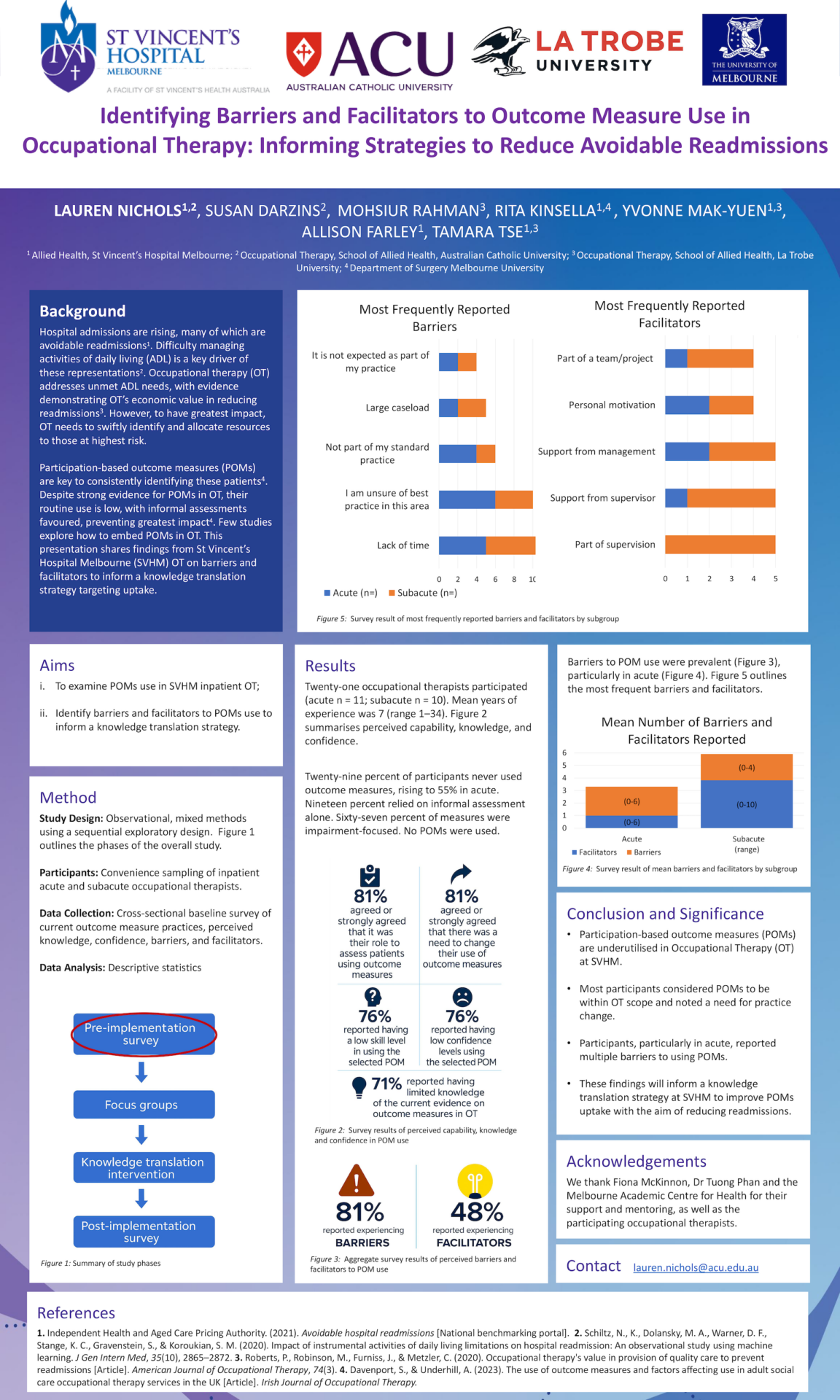
In this context, Lauren Nichols, a senior occupational therapist at St Vincent’s Hospital, Melbourne and Western Health, examined how allied health teams identify patients at highest risk of avoidable readmission and whether participation based outcome measures could support more consistent, higher value clinical decision making.
The first stage of the study mapped barriers and facilitators to change across the occupational therapy team. Staff recognised the value of change and reported strong peer support, while limited time, high referral volumes, and discomfort with withdrawing from low value activity influenced practice. These findings informed a second stage evaluating targeted interventions to increase use of a participation based outcome measure and assess its potential to identify patients at highest risk of readmission.
Linking local improvement efforts to system learning: reflections from the International Forum
Presenting her work at the International Forum on Quality and Safety in Healthcare in Canberra, Australia, broadened Nichols’ perspective on how local improvement efforts connect to wider systems change. The Forum was her first quality and safety meeting, and it exposed her to shared challenges across disciplines, sectors and countries.
Nichols described the immediate effect of the opening plenary:
“It talked about that tiny iteration and how you work towards a bigger picture. It definitely triggered in me what the bigger picture might look like outside of my setting.”
Nichols is completing the second stage of the project, which focuses on increasing uptake of participation based outcome measures to establish a consistent dataset across teams. This phase aims to address behavioural and organisational barriers to routine use, recognising that reliable data are a prerequisite for further analytical work.

Coming to the Forum has created some connections outside of just occupational therapy… I have had the opportunity to talk about where this sits outside of occupational therapy with leaders in health care and other disciplines as well.
Lauren Nichols
Senior occupational therapist, St Vincent’s Hospital, Melbourne and Western Health, Australia
Nichols’ findings have implications for allied health services operating under sustained demand and constrained staffing. More consistent use of participation based outcome measures may support safer patient selection, reduce low value activity, and enable clinicians to direct time and expertise towards patients at greatest risk of avoidable readmission. This approach aligns with national workforce priorities that emphasise full scope practice as a mechanism to improve efficiency and care quality.